A previous version of this bill has been passed in Nebraska.
Download Model Bill in Word.docx format
See supporting fact sheets and affidavits here or download Word copy here.
The
list of risk factors in section 3 is mostly taken
verbatim from the 2008 report of the APA Task
Force on Abortion and Mental Health.
Prevention of Coerced and Unsafe Abortions Act
Be it enacted by the General Assembly of
this STATE, as follows:
Section X, Chapter X (governing medical negligence or
informed consent), is amended by adding thereto one new
section, to be known as section New SECTION, to read as
follows:
Section 1. Name of Act and Legislative Findings
This section shall be known and may be cited as the "Prevention of Coerced and Unsafe Abortions Act" [or the "Negligent Pre-Abortion Screening Act”].
The Legislature hereby finds and declares:
- Many women feel pressured into unwanted abortions which violate their moral beliefs, maternal desires, and expose them to heightened rates of emotional distress and psychological illness.[1]
- Medical research has demonstrated that certain subgroups of women who are at higher risk of experiencing negative reactions associated with abortion can be identified by screening for pre-existing risk factors, including, but not limited to, the perception of feeling pressured to have an abortion, a prior history of mental illness, negative moral beliefs about abortion, and other statistically significant risk factors.[1]
- Women who feel pressured into unwanted abortions are at increased risk of “defective decision making,” as described by Uta Landy, a former executive director of the National Abortion Federation.[2] As a result, many women have a high degree of ambivalence about abortion, some are swayed to abort by others against their own preferences, and some will almost immediately regret undergoing or starting the abortion process.[1]
- Abortion has few, if any, medical benefits[3] but numerous and significant risks,[1,3–5] including “sadness, grief and feelings of loss….and some experience clinically significant disorders”[6] post-traumatic stress disorder[7–9], increased risk of subsequent reproductive health problems[10,11], rapid repeat pregnancies,[12] and cardiovascular disease.[13]
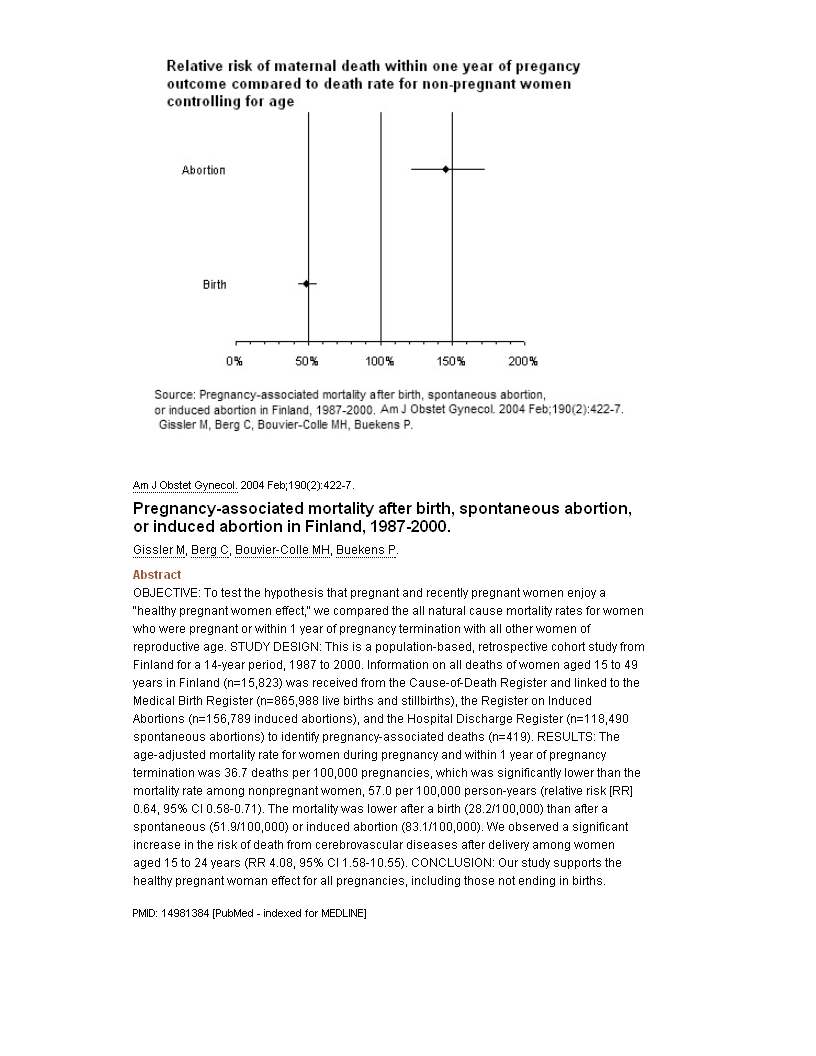
- Abortion is also linked to an elevated risk of premature death from both suicide and natural causes.[14] False claims that abortion is safer than childbirth are based on apples to oranges comparisons.[15] In fact, 100 percent of studies using the same measuring stick for both abortion and childbirth (linkage of death certificates to records of reproductive care) have shown that abortion is always linked to a higher risk of a woman’s premature death than childbirth.[16] There is even a dose effect, with each exposure to abortion increasing the risk of premature death by approximately 50 percent.[17]
- Whenever allowed by law, abortions should only occur when they are most likely to benefit a woman’s health. Even in the most dire circumstances, women deserve the highest quality of medical care, including (a) adequate pre-abortion screening, (b) full disclosure of all statistically associated risks, and (c) an evidence-based, reasonable medical recommendation based on the patient’s own individual risk versus benefits profile.[4]
- Research examining women’s preferences for disclosure of risks reveals that women prefer complete disclosure, even of infrequent and less serious complications associated with elective medical procedures, including abortion.[18]
- Historically, many abortion providers have withheld information about statistically significant risks associated with abortion. However, this paternalistic screening of risk disclosures was rejected in Planned Parenthood v. Rounds as an unjustified departure from normal medical standards.[19]. Citing FDA rules requiring full disclosure of all risks that are statistically associated with medical treatment even if a direct causal relationship has not been proven (21 C.F.R. § 201.80(e)), the 8th U.S. Circuit Court of Appeals (en banc) has affirmed the right of women to full disclosure of all risks statistically associated with abortion.
- Inadequate pre-abortion screening, counseling and risks disclosure may have been, and is at continued risk of being, fostered by financial and ideological conflicts of interest. There are individuals and organizations who seek to increase abortion rates as a means of population control and social engineering even at the expense of women, especially among the most disadvantaged and vulnerable populations.[20–22]
- These advocates for increasing abortion rates have a history of concealing or understating the risks associated with abortion, exaggerating its presumed benefits, failing to provide adequate pre-abortion screening, and have even engaged in obstruction of women’s efforts to stop or reverse abortions by removal of laminaria or prescription of antidotes for mifepristone.[4]
- Given the conflicts of interest that are often attached to abortion counseling, and the history of inadequate screening and disclosure of risks, it is a service to the health of women to define at least the minimum standards of care for pre-abortion screening and counseling in statute.
- It is within the resources of organizations such as Planned Parenthood of America, the National Abortion Federation, and the American College of Obstetrics and Gynecology to conduct systematic literature reviews to maintain and update checklists of all statistically significant risk factors and abortion associated risks that have been reported in peer reviewed literature. It is also within their means to provide such information in the form of printed or computerized checklists to facilitate pre-abortion screening and for full disclosures of all risks that may be relevant to a reasonable patient in accord with each patient’s own individual risk profile.
- The problem of reducing health care costs, as addressed by U.S. Preventive Services Task Force initiative, is centered on promotion of evidence-based medicine. This evidence-based approach underscores the importance of avoiding medical procedures that either (a) have been shown to not produce the positive effects sought by the patient or (b) produce negative health effects which are greater than the likely benefits. The standards of evidence-based medicine can be applied to abortion recommendations.
- It is the ethical responsibility of health care providers who provide or refer for abortion to provide pre-abortion screening and counseling of a high-quality sufficient to identify and avoid unsafe, unnecessary and/or unwanted abortions, and conversely to ensure that abortions are only done when there is a reasonable evidence-based medical determination that the likely benefits are substantially greater than the risks.[4] It is the intent of this statute to attach legal responsibilities to these ethical responsibilities.
- The fastest growing method of abortion is via mifepristone prescriptions. At least some portion of women who ingest mifepristone change their minds and wish to stop the abortion. The immediate ingestion of progesterone can act as an antidote that will cancel the effects of mifepristone and may help save a woman’s pregnancy. A state mandate requiring inclusion of progesterone in all mifepristone prescriptions will save at least some lives and will protect and enhance women’s reproductive choices.
- Collection of data regarding the frequency of women being pressured into abortions and the frequency and distribution of other risk factors may contribute to improved medical care and public health policies.
- In order for the Department of Health to (a) accurately track abortion associated deaths and investigate and develop more accurate maternal mortality reports, (b) to investigate pregnancy associated complications, suicides and other negative outcomes associated with abortion, (c) to provide services associated with pregnancy loss care, such as those in Finland which provide post-abortion suicide assessments and counseling, and (d) to investigate the reasons for abortion and the prevalence of risk factors among those who have abortions, it is necessary to implement an Abortion Registry with appropriate safeguards of patients’ identifying information.
- Promoters of unsafe abortions, whether for financial or ideological reasons, pose a real threat to women’s health. This threat can be mitigated by expanding the rights to redress against any organization or person who is not a licensed physician who attempts or completes an abortion on a pregnant woman, or who aids, abets, enables or encourages the commission of a self-induced abortion.
Section 2. Definitions
As used in this section, the following terms mean:
(1) "Abortion" means the use or prescription of any instrument, medicine, drug, or other substance or device intentionally to terminate the pregnancy of a woman known to be pregnant with an intention other than to increase the probability of a live birth, to preserve the life or health of the child after live birth, or to remove a dead unborn child, and which causes the premature termination of the pregnancy;
(2) "Abortion provider" means any physician or entity that performs or provides abortions or refers for abortions as a normal part of their business at least ten times per year;
(3) "Complications associated with abortion" means any adverse physical, psychological, or emotional reaction that has been shown to be significantly associated with abortion.
(4) "Medical emergency" means that condition which, on the basis of the physician's reasonable clinical judgment, so complicates the medical condition of the pregnant woman as to necessitate an immediate abortion to avert the death of the mother or for which a twenty-four-hour delay will create grave peril of immediate and irreversible loss of a major bodily function;
(5) "Negligible risks" means risks that a reasonable patient would consider to be immaterial to a decision to undergo an elective medical procedure;
(6) "Physician" means any person licensed under [List statute number here] to practice medicine in this state, including medical doctors and doctors of osteopathy;
(7) "Qualified person" means a licensed physician or an agent of the abortion provider who is a licensed psychologist, licensed social worker, licensed professional counselor, or licensed registered nurse;
(8) "Relative risk rates" means any statistically significant relative risk rate or odds ratio for any adverse physical, psychological, or emotional reaction significantly associated with abortion.
(9) “Risk factors” means any factors, including any physical, psychological, emotional, demographic, or situational factor significantly associated with abortion and one or more complications associated with abortion.
(10) “Self-induced abortion” means any abortion or menstrual extraction attempted or completed by a pregnant woman on her own body without a prescription from a licensed physician.
(11) “Significantly associated with abortion” means any physical, psychological, emotional, demographic, or situational factor for which there is a statistically significant association with abortion such that there is less than a five percent probability (P < .05) that the identified statistical association is due to chance, and the finding of the statistically significant association has been published in English not less than twelve months prior to the day of a patient’s pre-abortion screening in a peer-reviewed journal indexed by the United States National Library of Medicine's search services (PubMed or MEDLINE), or the index PsychInfo, or in any journal included in the Thomson Reuters Scientific Master Journal List.
Section 3. Negligent Pre-Abortion Screening and Counseling
In addition to any other requirements under state law, it is an act of medical negligence to perform or refer for an abortion, except in the case of medical emergency, within the State or on a resident of the State unless all of the following are true:
- At least one hour prior to the performance of an abortion, a person licensed under the Uniform Credentialing Act as either a physician, psychiatrist, psychologist, mental health practitioner, physician assistant, registered nurse, or social worker has:
- Evaluated the pregnant woman in person to identify the presence risk factors associated with complications associated with abortion, the list including, at least the following risk factors[6]:
- perceived pressure from others to terminate a pregnancy;
- perceived opposition to the abortion from partners, family, and/or friends;
- lack of perceived social support from others;
- low self-esteem, a pessimistic outlook, low-perceived control over life;
- a history of mental health problems prior to the pregnancy;
- feelings of stigma;
- perceived need for secrecy;
- use of avoidance and denial coping strategies;
- feelings of commitment to the pregnancy;
- ambivalence about the abortion decision;
- low perceived ability to cope with the abortion prior to its occurrence;
- abortion after the first trimester;
- a history of prior abortion or miscarriage;
- the woman views an abortion to be in conflict with her personal or religious values;
- the woman is twenty-two years old or younger;
- a family history of breast cancer;
- a history of cardiovascular disease, diabetes, or hyperlipidemia;
- any other risk factors identified by the Department of Health;
- any other risk factors that are known or should have been known by an abortion provider who keeps abreast of the published literature, and
- Informed the pregnant woman and the physician who is to perform the abortion of the results of the evaluation in writing, including a complete description of all complications associated with abortion and of all complications associated with each identified risk factors associated with the woman’s own risk factor assessment, with the descriptions of complications including incident rates and visual depictions of the range, or at least the highest published incidence rates, for each complication associated with abortion and the relative risk rates as compared to women who continue the pregnancy, are not pregnant, have miscarriages, carry an unplanned pregnancy to term, and any other published group for comparison;
- Prepared a written evaluation including, at a minimum, the age of the woman, the stated reason or reasons for requesting the abortion, a copy of the checklist in subsection (1)(a), a description of any perceived pressures identified in subsection (1)(a) in a manner that does not reveal any personal identifying information, and the licensed person's written certification that the pregnant woman was fully informed of and understood her relevant risk factors and the complications associated with abortion; and
- Retained a copy of the written evaluation results in the pregnant woman's permanent record, with said copy including the woman's written certification that she personally discussed and understood the risk factors and any associated complications with the licensed person who signed the written certification.
- Evaluated the pregnant woman in person to identify the presence risk factors associated with complications associated with abortion, the list including, at least the following risk factors[6]:
- After review of the written evaluation in subsection (1), the physician performing the abortion has formed a reasonable medical judgment, documented in the permanent record and disclosed in person to the woman at least one hour prior to performing the abortion, that the preponderance of statistically significant peer reviewed studies indicates that:
- The physical and psychological risks associated with abortion for patients with risk factors similar to the patient's risk factors are negligible risks; or
- Continuance of the pregnancy would involve greater risk of injury to the physical or mental health of the pregnant woman than if the pregnancy were terminated by induced abortion; or
- Continuance of the pregnancy would involve less risk of injury to the physical or mental health of the pregnant woman than if the pregnancy were terminated by induced abortion.
- A digitally signed copy of the electronic file, including all information from subsections (1) and (2), is filed with the Department of Health’s Abortion Registry within thirty days after the abortion and a copy is retained in the physician’s permanent records.
Section 4. Civil Remedies.
- In addition to other remedies available under state law, the intentional, knowing, or negligent failure to comply with the requirements of Section 3 shall provide a basis for the following:
- Each violation of this Section 3 shall entitle the woman or her survivors to ten thousand dollars for each failure to screen for a risk factor and for each failure to inform her of associated complications plus actual damages and reasonable attorney's fees and costs;
- Recovery for the mother and/or father of the aborted child of damages for the wrongful death of the unborn child action under section <identify section number here>, whether or not the unborn child was viable at the time of the abortion.
- Recovery of attorneys’ fees and punitive damages under the deceptive business practices act <identify section number here> and for reckless endangerment <identify section number here> by any party showing by a preponderance of evidence:
- that the advertising and/or offering of abortion services to any residents of the State fails to fully disclose all risk factors and complications associated with abortion, and/or
- that the plaintiff sought an abortion and the abortion provider offered or recommended an abortion or abortion referral without first complying the requirements of section 3, even if an abortion was not undertaken or completed, and/or
- the manufacturer or distributor of abortifacients, including mifepristone, failed to notify all potential users of all risk factors and complications associated with abortion, and/or failed to provide adequate safeguards to ensure that physicians prescribing or distributing their abortifacients comply with the requirements of section 3.
- Any action for civil remedies based on a failure to comply with the requirements of section 3 shall be brought no later than the longer of:
- ten years after seeking an abortion, or
- four years after the date the woman becomes or should have been aware that the abortion was a probable or contributing cause of a physical or emotional complication, or
- four years after the woman has recovered from any physical, emotional, or psychological complications which may have impeded her ability to seek or cooperate with counsel in pursuit of her civil remedies.
- Notwithstanding the provisions of subsection (2) of this section, in the case of a woman who has died within one year of the abortion, any action under this section shall be brought by her survivors within two years of her death.
- Any party advertising abortion services or abortion referrals viewable to residents in the State shall be deemed to be transacting business in this state pursuant to section (example: Nebraska 25-536) and shall be subject to the provisions of this Act;
- Any resident of the State shall have standing to sue under this statute even if the abortion(s) occurred outside the state and/or prior to residency.
- The failure of an out-of-state abortion provider to complete and file the abortion registry form pursuant to section 5 shall create the presumption of an admission of medical negligence, reckless endangerment, and deceptive business practices.
- In any civil action involving Sections 3 or 5:
- In determining liability and validity of consent, the failure to comply with the requirements of Section 3 shall create the presumption that the plaintiff would not have undertaken the abortion if Section 3 been complied with by the physician;
- The absence of physical injury shall not preclude an award of noneconomic damages including pain, suffering, inconvenience, mental suffering, emotional distress, psychological trauma, loss of society or companionship, loss of consortium, injury to reputation, or humiliation associated with the abortion;
- The fact that a physician does not perform elective abortions, or has not in the past, shall not automatically disqualify that physician from being an expert witness. A licensed obstetrician or family practitioner with experience helping women in resolving pregnancy-related medical matters shall presumptively be qualified to testify as an expert on the screening, counseling, management, and treatment of unwanted or problem pregnancies;
- The failure to comply with the requirements of Sections 3 or 5 of this Act shall create the presumption that the negligence was willful and wanton unless the defendant proved by a preponderance of evidence that a lesser mental state in fact applied;
- Any waiver of the evaluations and notices provided for in Sections 3 and 5 of this Act is void and unenforceable;
- The Department of Health’s abortion registry form, Section 5(a), is intended to only establish minimum standards for reporting purposes. The absence of risk factors on the Abortion Registry form that are known or should have been known by the abortion provider does not bar plaintiffs from recovery of damages associated with these unlisted risk factors.
- It shall be an affirmative defense to allegations of inadequate disclosure under the standards and requirements of Section 3 that the defendants omitted the contested information because:
- Statistically validated surveys of the general population of women of reproductive age, conducted within three years before or after the contested abortion, demonstrates that less than five percent of women would consider the contested information to be plausible and relevant to an abortion decision; or
- In the reasonable medical judgment of two licensed psychiatrists who examined the patient within one month prior to the abortion, disclosure of the contested information would most likely have been the immediate and direct cause of a severe adverse effect on the physical health of the patient.
- It shall be an affirmative defense to allegations of inadequate screening under the standards and requirements of Section 3 that the defendants failed to screen for the contested information because no peer reviewed study was published after 1973, in the English language, in a journal indexed by the United States National Library of Medicine's search services (PubMed or MEDLINE) or the index PsychInfo, showing that alleged indicators and contraindicators, and risk factors are significantly associated with complications associated with abortion, wherein the statistical test for a significant association being such that there is less than a five percent probability (P < .05) that the reported association was due to chance.
- If the physician provided a minor patient with an abortion without the informed consent of the minor's legal guardian, the burden of proving that the minor woman was capable of maturely and independently evaluating the information given to her in the disclosure process, that the minor woman was capable of making a voluntary and informed choice, and that all aspects of the screening and disclosure were adequate shall fall upon the abortion provider.
- In addition to the other remedies available under common or statutory law of this state, a woman or her survivors shall have a cause of action for reckless endangerment and wrongful death against any person who recommends, attempts or completes an abortion or aids or abets the commission of a self-induced abortion, with the exception of a person who is a licensed physician or a licensed pharmacist filling a prescription.
- Proof of injury shall not be required to recover an award for reckless endangerment under this subdivision and the minimum award of damages for reckless endangerment shall be eight hundred thousand dollars, plus reasonable costs and attorneys’ fees.
- Damages for wrongful death of the aborted child shall be awarded when the preponderance of evidence shows that the defendant’s actions contributed to an abortion that was completed.
- The statute of limitations for suits brought under this subsection is 100 years.
- [Note: Consider if this subsection should be treated as it’s own separate section.]
Section 5. Abortion Registry
- The Department of Health and Human Services shall prepare, maintain, and periodically update an internet-based abortion registry form which shall be used for the reporting of every abortion performed in this State or elsewhere on residents of this State. The abortion registry shall include the following items:
- The age of the pregnant woman;
- The location of the facility where the abortion or medical treatment was performed;
- The name of the attending physician;
- The pregnant woman's complete obstetrical history regarding the year and outcome of all previous pregnancies (abortions, natural losses and live births);
- The stated reason or reasons for which the abortion was requested;
- A Likert-scale rated checklist of all risk factors associated with abortion;
- The attending physician’s medical recommendation as described in section 3(2);
- The zip code of the pregnant woman's legal residence;
- The woman’s name, birth date, place of birth and any other information the Department deems necessary for automated linkage to death certificates;
- Whether or not the abortion was in fact performed, the type of procedure performed, any complications or multiple pregnancies, and whether any secondary procedures were necessary to complete the abortion;
- Whether or not the woman returned to the clinic for the scheduled follow up(s);
- Not less than five and no more than twenty research questions, developed by the Department of Health and annually reviewed in consultation with researchers, which may be useful to better understanding the following subjects:
- the reasons motivating abortion;
- the prevalence of risk factors associated with abortion;
- the prevalence of complications associated with abortion relative to exposure to previous abortions;
- whether abortion screening provisions are successfully reducing the occurrence of unwanted or unsafe abortions.
- The electronic form shall be completed and electronically signed by the attending physician within thirty days after an abortion is performed. In cased of medical emergency, when an abortion was performed prior to the detailed risk assessment otherwise required in section 3, the abortion registry form must be subsequently completed by the attending physician, and the patient if accessible, to the best of the physician’s knowledge.
- The electronic form shall be completed and electronically signed by abortion provider staff after a woman has completed the screening process but an abortion was not performed, at least to the abortion provider’s knowledge, within thirty days after the woman has refused or been refused an abortion, or has failed to return for an abortion.
- An identical version of the electronic form shall be made available to the general public for self-evaluation, but such submissions shall not be electronically signed.
- Automated submissions of the form to harass or mislead the Department shall be a Class ?? felony.
- Completed forms shall be submitted to a secure server maintained by the Department of Health.
- Personal identifying information on the abortion registry form shall be confidential and shall not be revealed except upon the order of a court of competent jurisdiction.
- Personal identifying information on the abortion registry form shall not be disclosed or admissible in any criminal investigations or prosecutions against the patient seeking or undergoing an abortion.
- Disclosure, or unauthorized use, or unauthorized accessing of personal identifying information associated with the abortion registry is a Class ??? felony.
- The electronic form completion process shall provide users with a means to print copies of the form, including a unique identifier, that can be provided to the patient and retained in the physician’s permanent records.
- Out of state abortion providers who refer or provide abortion services to residents of the State are obligated to (a) complete the abortion registry form for any resident of the state seeking their services and (b) to provide a level of screening and counseling equal to or exceeding the requirements in Section 3.
- The Department of Health shall prepare annual reports based on the abortion registry, including:
- A report on the prevalence of risk factors reported by women seeking abortions that were performed and women seeking abortions that where not performed;
- A report on pregnancy associated deaths (defined as the death of a woman during or following a pregnancy) with a breakdown of the number of deaths from the five most common causes of death for each pregnancy outcome subgroup (birth, induced abortion, natural loss) based on record linkage of death certificates to the abortion registry, birth certificates, and any accessible fetal death certificates associated with natural losses. The annual report shall include pregnancy associated death rates within 42 days, six months, one year, and yearly cumulative rates through at least 5 years, and any additional time frames the Department deems informative.
- The Department shall make non-identifying information from the abortion registry available for research purposes, provided the researchers shall sign a non-disclosure agreement precluding the use of the written evaluations to attempt to use the non-identifying information to investigate or identify any individuals and notifying the researchers of the felony penalties associated with any such unauthorized use or disclosures.
- Researchers who have used the data in published peer reviewed papers shall be included among the consultants the Department shall poll on at least an annual basis for revision of the forms to further investigation of the four research areas described in subsection (4)(l).
Section 6. Construction.
(1) Nothing in this section shall be construed as creating or recognizing a right to abortion.
(2) It is not the intention of this section to make lawful an abortion that is otherwise unlawful or to make unlawful an abortion that is otherwise lawful.
(3) Nothing in this section shall be construed as defining the standard of care for any medical procedures other than induced abortion.
(4) A violation of Section 3 or 5 shall not provide grounds for any criminal action or disciplinary action by any State agency or State licensing authority against the physician or persons acting under the physician's direction or against a licensed medical facility, hospital, health care facility, or parent corporation of the health care facility.
Section 7. Severable.
If any portion of this act is enjoined and subsequently upheld, the statute of limitations for filing civil suit under this section shall be tolled during the period for which the injunction is pending and for four years thereafter.
Section 8. Abortion Information Depository (optional)
The Department of Health and Human Services shall make available on its Internet web site an Abortion Information Depository which shall include, in both an HTML format and in a downloadable portable document format (pdf), the information described in this section.
The Department is not required to engage in a proactive search for studies described in this section, but shall be required to maintain an updated list of information based only on qualified studies meeting the required definitions for inclusion which have been submitted for inclusion by third parties.
A qualified study is one which has been published in the English language in a peer-reviewed journal indexed by the United States National Library of Medicine's search services (PubMed or MEDLINE) or in any peer-reviewed journal included in PsycINFO after 1972, and which furthermore includes at least one finding that has been statistically tested finding such that there is less than a five percent probability (P < .05) that the identified statistical association is due to chance.
The Abortion Information Depository shall include directions for mailing the required information for nominating a qualified study and for submitting material summarizing qualified studies, and shall also provide a means for interested persons to nominate studies or submit summary materials by electronic submission process.
Nominations and submissions shall at a minimum include the complete citation and identification of at least one statistically significant risk factor or at least one statistically significant relative risk in order to assist the Department in determining if the minimum standards for inclusion are met. The electronic submission process shall also include an option for submitting a hyperlink to the study or an abstract of the study, or for uploading a copy of the published study.
Within 30 days of receiving a third party submission, the Department shall attempt to notify the third party either that the submitted citation has been added to the appropriate online bibliographic listing or shall be given notice regarding which of the conditions for qualifying studies were not met.
The Abortion Information Depository shall include:
(1) A bibliographic listing of all qualifying
studies, including any provided hyperlinks to
the abstract or complete study, provided the
link does not violate copyright law.
(2) Copies of
any documents submitted to the
Abortion Information Depository that include a
forest plot
of statistically significant (p<.05) relative risk rates of abortion
from qualified studies, with a
citation to the study reporting each relative
risk rate, a true and accurate description of each risk and the
population sample to which the reported risk
rate applies, and optionally a copy of the
abstract(s) of the qualified studies relied
upon.
(3) A copy of the informed consent material prepared under the State's informed consents statute (if any).
(4) A listing of social services offering assistance to pregnant women.
Supporting Affidavits
Sworn Declarations of Abortion Patients - Including patients of Planned Parenthood and, or residents of Nebraska




